Chest Xray - Tuberculosis TB
It’s has been estimated that 2 billion people worldwide are infected with mycrobacterium tuberculosis, often to shorten tuberculosis, or simply TB. 2 billion is a lot of people, right? But even other infected that doesn’t mean that all these people have symptoms. The vast majority about 90 – 95% aren’t even aware that they are infected with TB, and this is because usually our immune system can contain it, such that it isn’t able to multiply and often remains latent or dormant, as oppose to active TB which usually contain symptoms and means it can be spread to others. If the host immune system becomes debilitated at some point on the road, like with aids or some other illness or a person as grow older, it can allowed to reactivate and basically wake up and becomes very serious specially when spreads throughout the body.
Microbacterium are interesting batch there’s slender rod shape and need oxygen to survive, in other words their strict aerobes. They’ve got an usually waxy cell walls which is mainly a results the production of mycolic acid, because of this waxy cell wall they are acid fast, meaning that they can hold on into a die in spite of being expose to alchohol. Living in a bright red color seeing on Ziehl-Neelsen stain. The wall also makes them incredibly hardy, and allows them to resist in weak disinfectants and survive on dry surfaces for months at a time.
Mode of Transmission
Microbacterial tuberculosis is usually transmitted via inhalation, which is how they gain entry into the lung. Now we breathe in all sorts of bacteria and viruses all the time, but we got a defences to take care most of them. For one, air that we breathe in is a turbulent in upper airways and dried most bacteria against mucus which then clear pretty quickly. Ultimately though TB can avoid the mucus traps and make it its way to the deep airways in alveoli, where we have macrophages which eats up foreign cells digest and destroy them. With TB they recognize foreign protein on their cell surface and phagocytize them or simply package them into the space called phagosome. With most cases the macrophage then fuses the phagosome with the lysosome which has hydrolytic enzyme that can pretty much breakdown any biochemical molecule. TB is tricky though, and once it is inside the macrophage they produces a protein that inhibits this fusion. Which allows micro bacterium to survive. It doesn’t just not survive though, it proliferates and creates a localize infection.
Primary Tuberculosis
When TB bacteria already proliferate and created a localize infection at this point the person has already developed a primary tuberculosis. Which means that they have sign of infection soon after being exposed to TB. Even though its sound bad, most people at in this stage are actually asymptomatic or maybe had a mild flu like illness. About 3 weeks after initial infection, cell mediated immunity kicks in and immune cells surrounds the side of TB infection, creating a granuloma essentially an attempts to wall off the bacteria and prevent it from spreading. The tissue inside the middle dies as a result, a process referred to as caseous necrosis which means cheese like necrosis, since the dead tissue is soft, white and looks a bit like cheese. This area of the dead tissue is known as the ghon focus. TB also gets the nearby hilar lymph nodes, either carried over by immune cells to the lymph or by direct extension by the ghon focus infection and causes caseation there as well, and together this caseating tissue and associated lymph node make up the characteristics ghon complex. Ghone complex are usually a subpleural and acquiring in the lower lobe of the lungs, the tissue that are encapsulated by the granuloma under goes fibrosis and often calcification, producing scars tissue that can be seen in chest xray, this calcified ghon complex is called the ranke complex. In some cases although a scar is left over the microbacterium is killed off by the immune system. In some other cases even though they are walled off they remain viable and are there for still alive, but there just dormant. If when a person’s immune system becomes compromise like with AIDS or with aging, the ghon focus can become reactivated and the infection could spread from one or both upper lobes of the lungs. Its though that this is because that oxigination is greatest in this area and TB being an arrow prefers areas of greater oxygenation right. Since there are previously expose the immune systems memory T cells quickly release cytokines to try and control the new outbreak, which forms more areas of caseous necrosis, this time its tends to cavitate or forms cavities, which can allow the bacteria to disseminates or spread through the airways in the pneumatic channels to other parts of the lungs which can cause bronchopneumonia, but it can also spread via vascular system and in fact almost every tissue in the body called the systemic miliary TB.
When TB spreads to other tissues it causes complications related to organs affected. Kidneys are commonly affected resulting in sterile pyuria or high level of white blood cells in the urine. It might also spread to meninges of the brain causing meningitis, the lumbar vertebrae causing the pott disease, the adrenal glands causing addision’s disease, liver causing hepatitis and cervical lymph nodes causing lymphadenitis in the neck also known as scrofula.
Testing for TB
Testing for TB often starts with Purified Protein Derivative or PPD intradermal skin test, sometimes known as the tuberculin skin test, mantoux test, or simply TB test. With this test the tubertuclin is injected between layers of the dermis. Tuberculin is a component of a bacteria and if the person is previously been exposed to TB the immune systems reacts the tuberculin and produces a small localize reaction within 48 to 72hrs. If the reaction creates a large enough area of induration rather than just redness it considered to be a positive test. Positive tuberculin test simply means that the patient has exposed at some point to TB. It doesn’t differentiate between active and latent disease. As an alternative to tuberculin skin test, there is also an inteferon gamma release assay (IGRA) which look for the evidences in blood with previously exposure to TB proteins, since this one is a blood test you don’t need to show up again to have a test read like you do it with the PPD, also the IGRA is more specific to TB, rather than other types of micro bacterial infection is unlikely to be positive as a result of having a BCG vaccine in the past, a vaccine that’s protect against TB, and this is a pretty useful features of IGRA’s since VCG vaccine is given to a lot of children around the world to prevent the dissiminated TB.
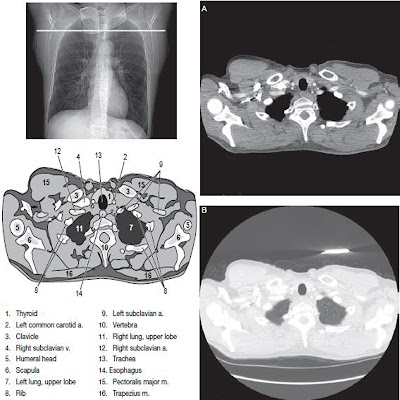
After doing a screening test with PPG or IGRA anyone with a positive results typically get a chest xray to look for a signs of an active TB disease. In patient with symptoms like fever, night sweats, weight loss and coughing up blood or hemoptysis. Its important collect samples from either in sputum or in bronchoalveolar lavage, which is where a bronchoscope is inserted through the mouth or the nose and into the lungs, fluid is squirted and that fluid is collected. This samples can now sents to lab for staining, culture and PCR to look for the evidence of microbacterium tuberculosis.
Treatment for TB
Treatment for latent TB infection typically involve using a single drug for prolong period of time. The most common approach is the isoniazid for 9 months. Treatment of active TB disease is typically a combination of antibiotics which results the patient will become non-infectious to others usually within a few weeks. Until that point though patients can spread TB to others and typically adults with reactivated TB that are the most infectious. As a result patients are typically keep in a negative pressure rooms and visitors are ask to wear a protective N-95 masks that cant filter out oil aerosols and for not resistant to oil, but can filter out atleast 95% of other aerosols in this case TB. Even after patients are no longer contagious, they typically kept on multiple medication for many months to be sure that the bacteria are being destroyed, usually with directly observatory therapy or DOT or somebody watches and confirms that they are taking the medications.
Additionally, there is an enormous worry about new drug resistant strains of TB their causing infection in various part of the word. You may hear about MDR TB or Muti-drug Resistant TB or even XDR TB which is extremely drug resistant TB, which are incredible hard to treat because they don’t die with the present in our usual antibiotics. The buttom line is that to get an effective treatment, its super important to make sure that the drugs are being used to work against this specific strains of TB, that multiple medication are used together to prevent the drug resistant from developing and that medication are used for the entire course of therapy so that all the micro bacterium of TB is killed off.








No comments:
Post a Comment