As mentioned earlier, many disease other than acute appendicitis may produce signs and symptoms indistinguishable from those of acute appendicitis. In situations for which a clear diagnosis of appendicitis cannot be made by the patient’s history, physical examination, and laboratory evaluation, radiologic testing particularly ultrasonography and CT can be useful.
Plain radiographs of the abdomen are frequently obtained as part of the general evaluation of a patient with an acute abdomen, but they are rarely helpful in diagnosing acute appendicitis. Barium enema is unreliable in the diagnosis of acute appendicitis and has been replaced by ultrasonography and CT scan.
Diagnosis of Appendicitis using Ultrasound
Ultrasonography is inexpensive and widely available, does not require contrast agents and poses no special risk to the fetus in pregnant patients. It is particularly well suited for evaluating right lower quadrant or pelvic pain in pediatric and female patients. However, the technique used to visualized the appendix, called graded compression sonography, is highly operator dependent. Some of the difficulties with ultrasonography are related to the fact that a normal appendix must be identified to rule out acute appendicitis. This is difficult in obese or very muscular patients or when there is an associated ileus that produces shadowing secondary to overlying gas filled loops of bowel.
Accuracy of ultrasound also decrease with retrocecal or pelvic locations of the appendix. In addition, the following scenarios can occur:
- A false positive scan can occur in the presence of periappendicitis from surrounding inflammation
- A dilated fallopian tube can be mistaken for an inflamed appendix
- Inspissated stool can mimic an appendicolith
Patient often complain of discomfort resulting from the transducer pressure during ultrasound evaluation
Despite these limitations, when institutions are comfortable with ultrasound for the evaluation of suspected appendicitis, ultrasonography continues to serve as the primary imaging study in children and in young or pregnant women.
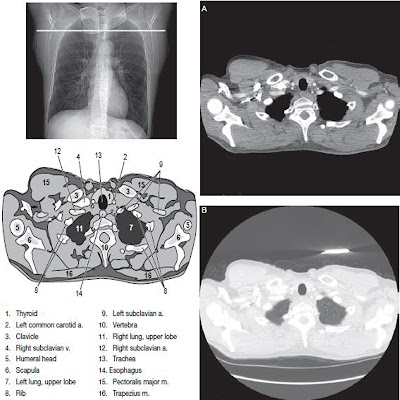
Appendicitis with CT scanning
CT is more accurate than ultrasonography, also because it is not as dependent on the skill and experience of the operator, CT scan is more reproducible from hospital to hospital. The diagnosis accuracy rate of CT for acute appendicitis is reported to range between 93% and 98&. Findings on CT increased the certainty of diagnosis more than findings on ultrasonography. Although ultrasonography is recommended as the initial imaging study in children, young woman and pregnant women, CT is most often recommended as the initial study in all other patients. In addition, CT Scan is recommended for patients in whom sonographic evaluation is suboptimal or indeterminate, or for those patients in whom perforation is suspected.
Comparison of Ultrasound and CT for Suspected Appendicitis
Ultrasonography Advantage
- The accuracy of the ultrasound study on appendicitis is between 71 to 91%.
- It is easily available
- Noninvasive
- No radiation
- Rapid
- No preparation needed
- Ability to diagnose other source of pain (especially gynecologic disorders)
Ultrasonography Disadvantages
- Highly operator dependent
- Not as accurate as CT Scan
- Difficult with large body habitus
- Cannot rule out appendicitis if appendix is not apparent
Computed Tomography Advantages on Appendicitis Diagnosis
- The accuracy of the CT scan study on Appendicitis is between 93 to 98%.
- More accurate
- Better identification of phegmon and abscess
- May complement ultrasonography when results are suboptimal
- Better ability to detect normal appendix
- Better at determining alternative diagnosis like ureter stone, diverticulitis and pancreatitis
Disadvantages of CT scan on Diagnosis of Appendicitis
- Radiation Exposure
- Patient discomfort/risk if contrast media is used
- More expensive then ultrasonography
- Not as good for gynecologic disorders
- Common CT scan findings in Acute Appendicitis
The most common CT findings in acute appendicitis are a dilated nonopacified appendix, soft tissue stranding or inflammation into adjacent periappendiceal fat and appendicolith.
 |
| common CT finding in acute appendicitis is a dilated nonopacified appendix (arrow). |
When the appendix is not seen, appendicitis is typically excluded if other signs of appendicitis are absent. In addition, CT scans are generally considered to be negative for appendicitis in the following scenarios:
- The appendiceal lumen fills completely with oral or rectal contrast material or air.
- The appendiceal lumen contains air and contrast material and the appendix is less than or equal to 6mm in maximum diameter.
- The appendiceal wall is less than 2 mm thick
- No periappendiceal inflammation is present.
Different investigation hace suggested different combinations of CT scan findings to obtain a definitive diagnosis of appendicitis. For example, Wijetunga and colleagues interpreted the CT scan as positive for appendicitis if 3 or more of the following criteria are present:
- The appendix is greater than 6mm is maximum diameter
- There is no contrast material in the appendiceal lumen.
- Inflammatory changes in the periappendiceal fat are present, like far stranding or phlegmon, extraluminal gas bubbles, fluid collection, or enlarged lymph nodes.
- Appendicoliths, 1 or more are present.
- Cecal wall thickening is present.
 |
| Appendicolith (white arrow) with surrounding inflammation (black arrows). |
 |
| A thickened appendix (white arrow) surrounded by abnormal inflamed fat (black arrows) is shown. |
Occasionally, patients with right lower quadrant pain will have CT scan images that show only one indication of appendicitis. In these situations, the radiologist may be uncertain as to whether appendicitis is present. Other researchers have diagnosed appendicitis solely on the basis of the present of an abnormal appearance of the appendix.







No comments:
Post a Comment